Best Corneal Transplant Surgery In D.N Nagar, Andheri, Mumbai
A corneal transplant is where the abnormal cloudy or scarred patient’s cornea is removed and a donor cornea (the clear window on the front of the eye, which has been obtained from someone who has donated their cornea) replaces the abnormal patient’s cornea. A corneal transplant (also known as a corneal graft) is only worth doing when the inside of the eye (retina and optic nerve) is still functioning well. The camera analogy is that there is no purpose in replacing the clear lens in the camera if the photographic components are not working. Conditions that may have damaged the inside of the eye are glaucoma, optic nerve disease, retinal detachment, severe inflammation or infection inside the eye.
There are two principal types of corneal transplant:
Partial thickness (or lamellar graft) or full thickness (or penetrating graft). Dr Ankita Patil will advise you of the type of transplant best suited to your condition.
1) Penetrating (full thickness) corneal grafts
Penetrating grafts have been the most widely carried out transplant for all types of corneal disease for over 40 years. However this type of graft is only mandatory if there is deep corneal scarring OR when the corneal disease involves both the endothelium AND the stroma.
The down side of a penetrating graft is that transplanting the endothelium may lead to rejection, which is the commonest complication of this type of graft (about 20% for low risk cases), and leads to graft failure in some. Also the donor endothelium has a limited lifespan.
2)Deep anterior lamellar grafts (DALK)
Deep Anterior Lamellar Keratoplasty (DALK) operations have become more widely used because of the benefits of reduced rejection and graft failure, and the development of better techniques for doing the surgery. Anterior lamellar grafts are only suitable for use in conditions affecting the front layer (epithelium) and central layer (stroma) of the cornea. A lamellar graft will not become “clear” if the posterior layer of the cornea (endothelium) is diseased or damaged. The down side is that the technique of deep anterior lamellar keratoplasty can be technically challenging, and if the endothelium is perforated during the surgery the vision may not recover without a penetrating graft. The surgeon can convert to a full (or penetrating) graft at the time if this happens.
Also the vision after a successful penetrating graft can be better than that following a successful lamellar graft, although the difference is small and patients can expect to meet the driving standard after both types. In a proportion of cases, the vision after an anterior lamellar graft is as good as with a penetrating graft.
3)DMEK (Descemets membrane endothelial keratoplasty)
DMEK is an endothelial graft containing only the delicate Descemet’s membrane and endothelium. DMEK is the newest method of surgery, which gives excellent rapid restoration of vision. However it can be associated with a higher rate of dislocation, necessitating more than one operation. The benefits of DSAEK or DMEK are a smaller operation for the eye compared to a penetrating graft, as the surgery is carried out through a keyhole incision, and requires only a few stitches to close the wound. This leaves the eye much stronger than after a penetrating graft, and also eliminates the problems of regular and irregular astigmatism that accompany all penetrating grafts. This speeds up the recovery period.
Risks and complications associated with corneal transplant surgery
- Dislocation of the transplant, necessitating a second operation to re-attach the graft, or a repeat DMEK.
- Corneal graft rejection
- Infection
- Primary donor transplant failure
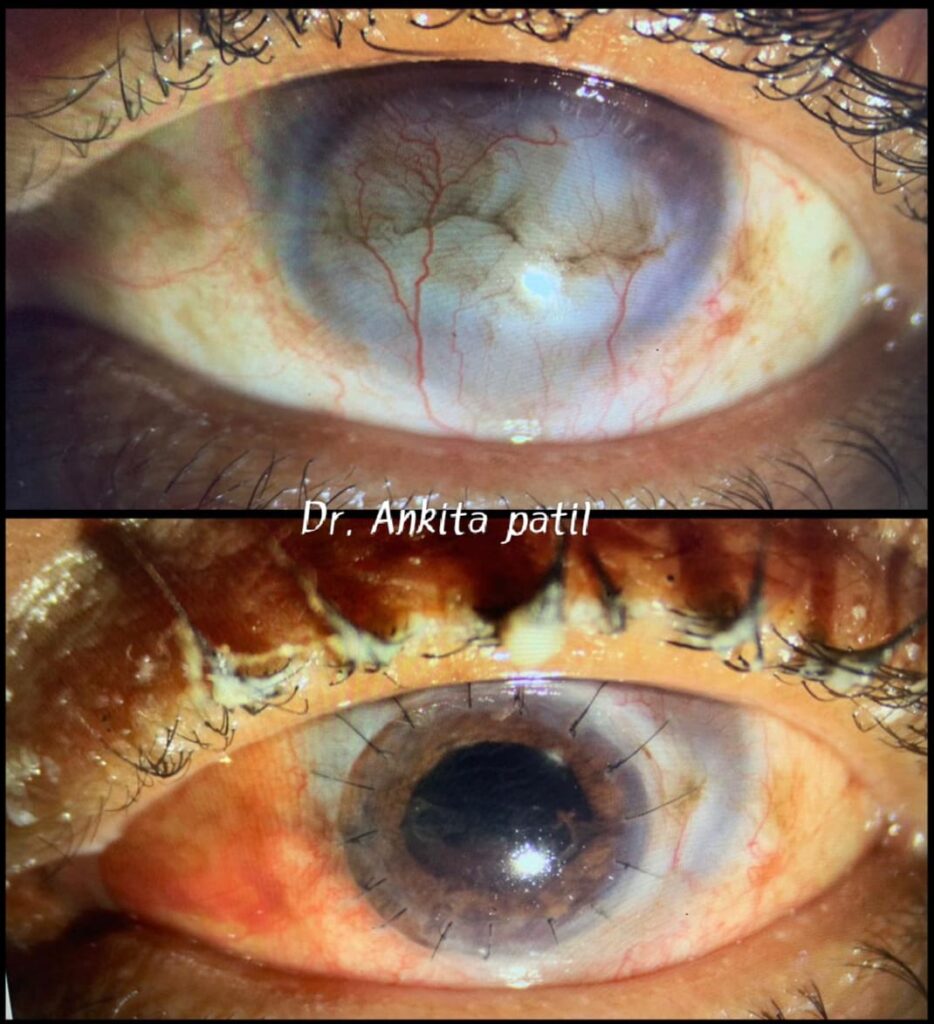
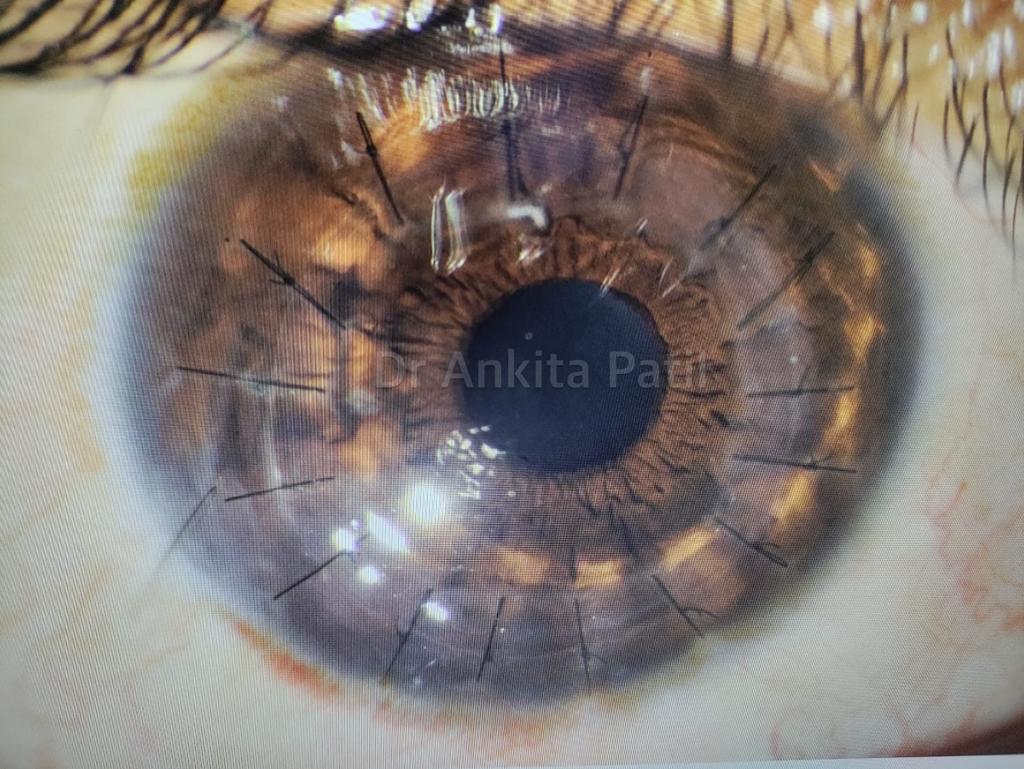
Post - Operative Result
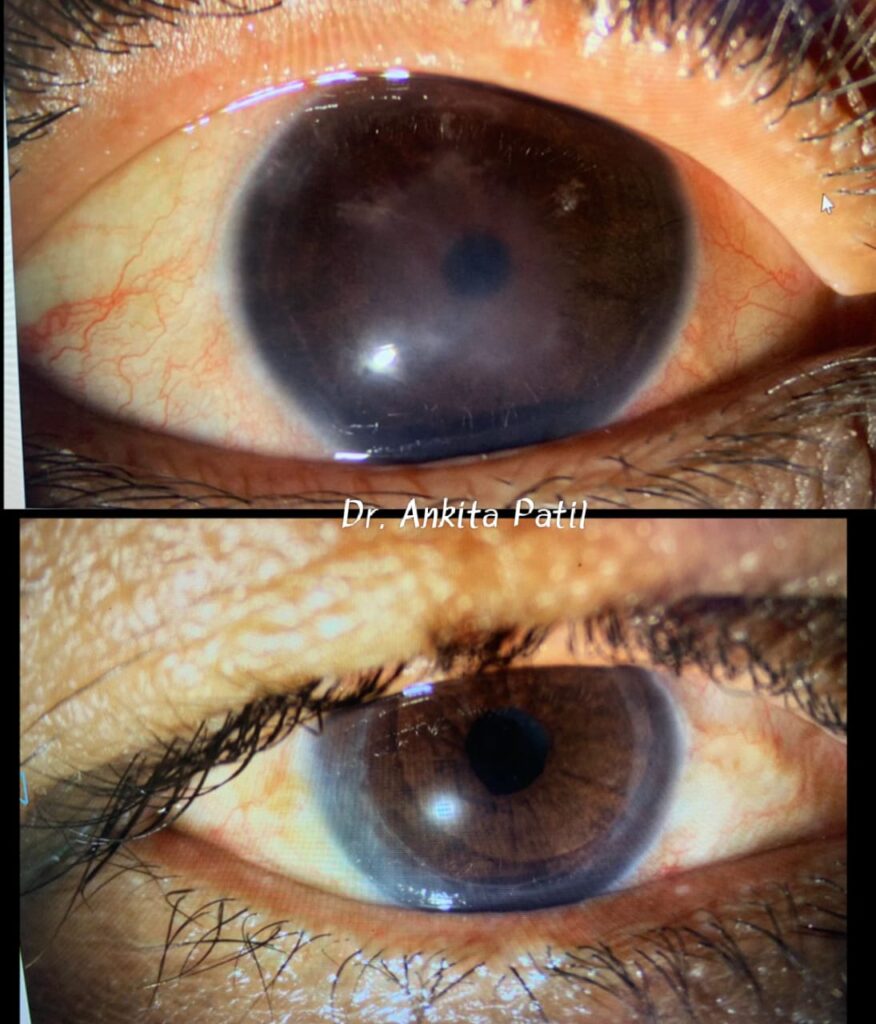
Lamellar Keratoplasty (DSEK)