Corneal Dystrophy
Corneal dystrophies are eye diseases that involve changes in the cornea (the clear front layer of your eye). These diseases usually run in families.
Corneal dystrophies
Most corneal dystrophies are progressive — they get worse over time. Some cause vision loss or pain, but some have no symptoms. The only way to know for sure if you have a corneal dystrophy is to get a comprehensive dilated eye exam. Your eye doctor will use a microscope with a bright light attached (called a slit lamp) to check your eyes for signs of corneal dystrophies.
Keratoconus
Keratoconus is usually diagnosed in teens and young adults. It causes the middle and lower parts of the cornea to get thinner over time. While a normal cornea has a rounded shape, a cornea with keratoconus can bulge outward and become a cone shape. This different cornea shape can cause vision problems.
Symptoms of keratoconus include:
- Itchy eyes
- Double vision
- Blurry vision
- Nearsightedness (when far-away objects look blurry)
- Astigmatism (when things look blurry or distorted)
- Sensitivity to light

As keratoconus gets worse, it may cause eye pain and more serious vision problems
Most people with keratoconus can correct their vision problems by wearing glasses, soft contact lenses, or special hard contact lenses that change the shape of the cornea. Your doctor may also recommend a procedure called corneal cross-linking to strengthen your cornea. If your keratoconus causes severe corneal scarring or you have trouble wearing contact lenses, you may need a corneal transplant.
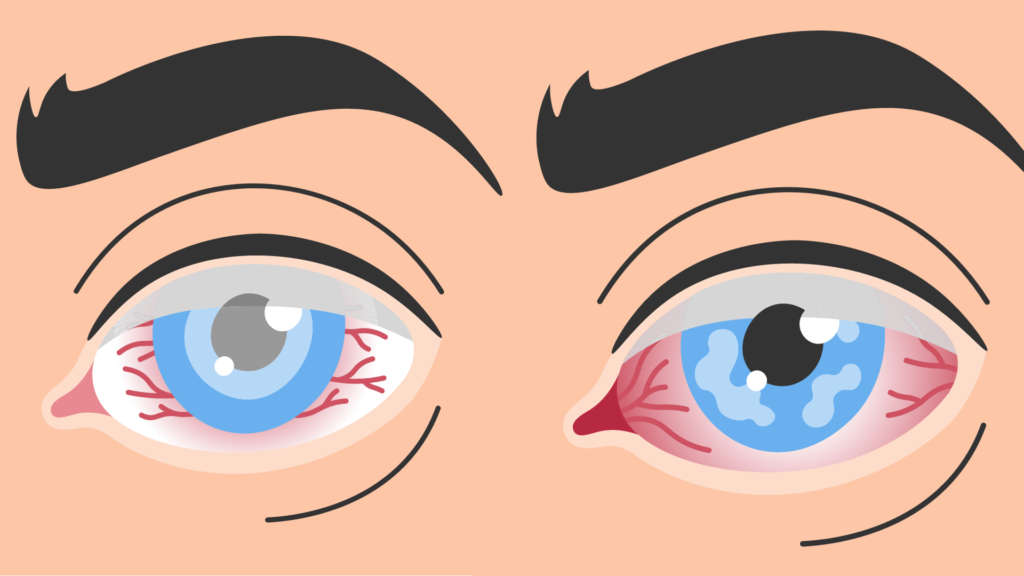
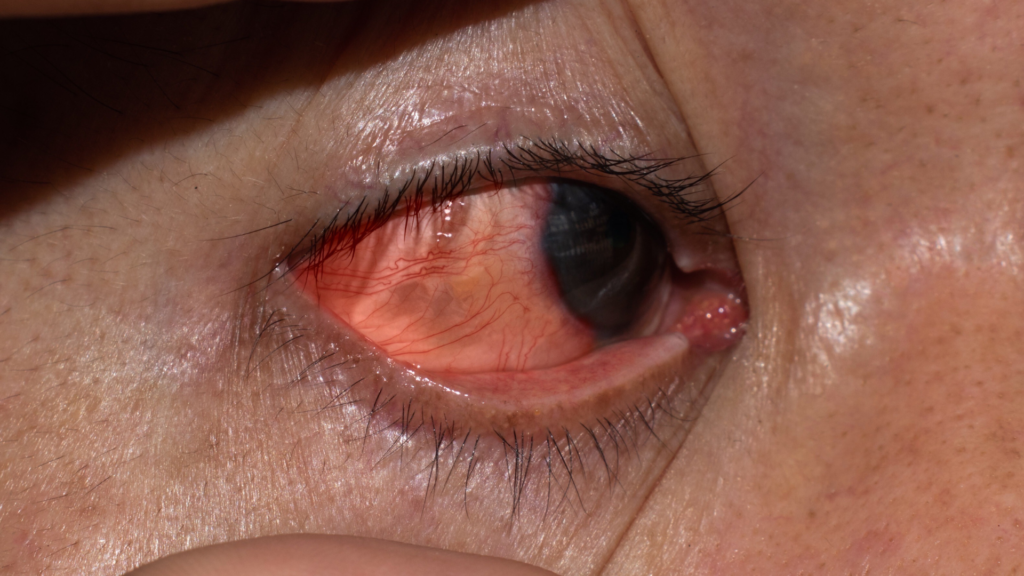
Corneal Ulcer
A corneal ulcer is an open sore on your cornea. Your cornea is the dome-shaped clear tissue layer that covers the front of your eye. Infection is the most common cause of a corneal ulcer.
Who gets a corneal ulcer?
You’re at risk of a corneal ulcer if you:
- Wear contact lenses, especially if you sleep in your contacts.
- Have or have had shingles, cold sores or chickenpox.
- Have dry eyes.
- Have eyelids that don’t close all the way.
- Use steroid eye drops.
- Have an injury or burn on your cornea.
- Have diabetes.
- Have had prior eye surgery.
- Have other eye diseases.
How common are corneal ulcers?
In the U.S., between 30,000 and 75,000 corneal ulcers occur each year. About 12% of all corneal transplants are done due to a corneal ulcer.
Is a corneal ulcer serious?
A corneal ulcer can cause permanent damage, even blindness if it’s not treated. If you think you have a corneal ulcer or have any eye problems that bother you, contact your eye care provider right away.
Limbal Stem Cell Deficiency
Treatment of LSCD
Therapeutic options for LSCD range from conservative to invasive and depend on the severity of the pathology. Conservative therapeutic options include supportive management, corneal scraping, and amniotic membrane patching. In these cases, recovery depends on the presence of some remaining LESCs that can be rehabilitated to restore the epithelium. If there are no remaining stem cell reserves, the cornea must be reseeded with new LESCs. Over the past 18 years, optimizing reseeding techniques has been a major focus of corneal tissue engineering. The earliest techniques required large sections of donor tissue either from the patient’s fellow eye (autograft) or from a healthy donor or cadaver (allograft).
Taking such large biopsies places the donor eye at risk of developing LSCD. In 1997, Pellegrini et al. reported the first application of ex vivo expansion of a very small stem cell biopsy in the treatment of LSCD. The ex vivo technique significantly reduced the risk to the donor eye. Since the original report, numerous clinical trials have reported outcomes of tissue engineered corneal surface reconstruction. This review will focus on the nature of LESCs and the evolution and optimization of cultivated limbal epithelial stem cell transplantation (CLET) as well as possible future directions.
Dry Eye
Signs and Symptoms
Ocular irritation is one of the earliest symptoms a patient with KCS may experience. Classically, the patient describes a sandy, gritty, foreign-body sensation, in one or both eyes, that often becomes more pronounced as the day progresses. Some patients may note a more severe “burning” sensation in the eye when exposed to particularly dry or irritating environments, such as dry heat, warm or smoke-filled rooms, and wind. Sensitivity to light may also be reported.
Diagnostic Tests:
- Vital Dye Stains
- Tear Break-up Time (BUT)
- Schirmer Tear Tests
Treatment
1)Artificial tears remain the primary treatment for mild to moderate keratoconjunctivitis sicca (KCS). Most artificial tears act as lubricants although others aim to replace missing tear constituents or to decrease the solute concentration in the tears.
2)Ointments offer the advantage of increased viscosity and retention time,but they may blur vision because of their increased viscosity. They are particularly helpful for use at bedtime or in individuals in whom the disease is more severe.
3)Cyclosporine
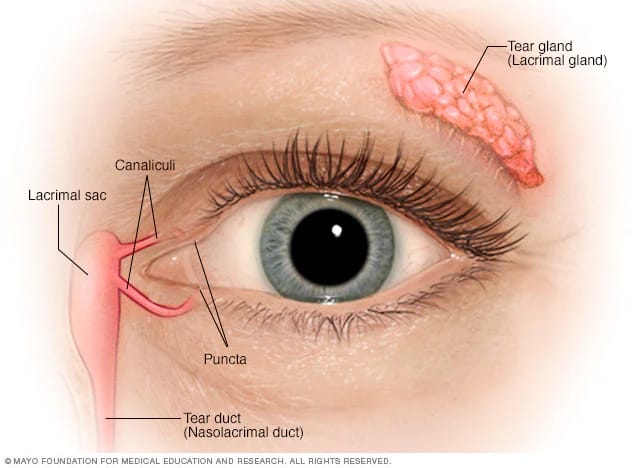
4)Tear Conservation by Punctal Occlusion
5)Partial or Total Tarsorrhaphy
6)Serum Tears
7)Treatment of Meibomian Gland Dysfunction